Ref: How to choose the best lateralization and distalization of the reverse shoulder arthroplasty to optimize the clinical outcome in cuff tear arthropathy by Philippe Valenti, MD, Frantzeska Zampeli, MD, PhD, Efi Kazum, MD, Carlos Murillo-Nieto, MD, Ahmad Nassar, MD, Mohamad K. Moussa, MD, MS
How to Choose Lateralization and Distalization of the Reverse Shoulder Arthroplasty to Optimize the Clinical Outcome in Cuff Tear Arthropathy
Optimizing implant related parameters on the outcome of reverse shoulder arthroplasty remains a topic of investigation. While there are many parameters affecting outcomes unique to the patient such as preoperative motion, bone integrity, cuff and deltoid muscle/tendon status, as well as prosthesis related factors, optimizing the surgeon-specific variables of implant positioning remain perhaps the most modifiable. This study included a cohort of 62 patients without substantial preoperative stiffness (categorized as purely cuff arthropathy) and attempted to identify implantation variables predictive of a favorable outcome, identified by an ASES score of 76 (the literature-identified patient acceptable symptom state). Analysis of two implant parameters, distalization and lateralization, resulted in significant observations.
Key Findings on Implant Distalization and Lateralization Angles (DSA and LSA)
The primary results of the study were that patients with favorable ASES scores (>76) had less lateralization of the implant (defined as a lateralization angle [LSA] of no more than 90.5 degrees) and higher distalization of the implant (defined as a distalization angle [DSA] of no less than 37.5 degrees). The calculation method for these angles is provided in the study but in brief terms:
- The LSA is the angle formed by a line drawn from the superior glenoid tubercle to the lateral acromion and another line from the lateral acromion to the lateral greater tuberosity. Higher LSA values indicate a more lateralized RTSA.
- The DSA is the angle formed by a line drawn from the lateral acromion to the superior glenoid tubercle and another line from the superior glenoid tubercle to the superior greater tuberosity.
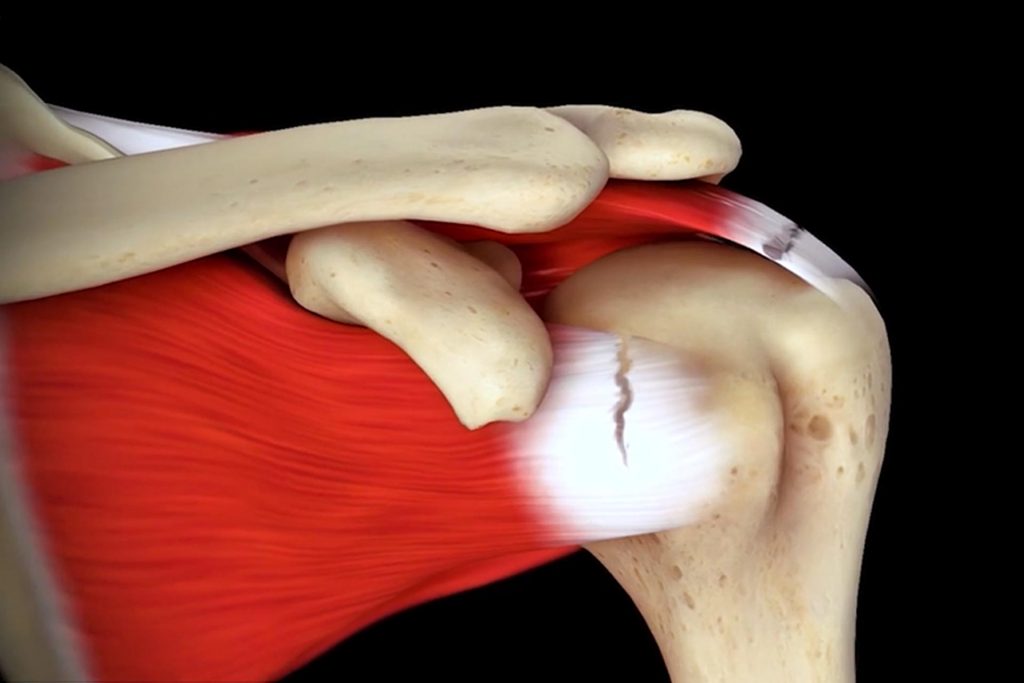
The authors identified fairly good predictive value of using the LSA and DSA in predicting the ASES score of the reverse arthroplasty (based on area under the curve in the receiver operator characteristic). The speculated reason that increased lateralization led to inferior outcomes was that the additional lateralization led to increased acromial stress and glenoid implant shear forces, as well as possible impingement between the greater tuberosity and the acromion. Regarding the distalization of the implant, it was shown that there were effectively no upper limits of DSA on outcome, meaning that the more distal the better, at least in this study.
Limitations of the Study and Implant Specificity
In my opinion, a limitation of the study was that some of the noted outcome parameters may be specific to the implant (as determined by the area under the receiver operator characteristic), and some of the deleterious effects of lateralization of the implant may not be seen with a medial glenoid design. In my practice I find the rate of acromial fracture is very low, and glenoid implant loosening is rare, underscoring the idea that these observations may not have occurred with a medial glenoid-lateral only humerus design such as the Equinoxe.
Clinical Recommendations for Reverse Shoulder Arthroplasty Planning
My goal is to optimize glenoid positioning by appropriately lateralizing and distalizing the implant to reduce the risk of notching, maximize impingement-free range of motion, and achieve sufficient soft-tissue tension to minimize instability. Achieving these goals is often consistent with the beneficial effect of distalization as seen in this study. One key takeaway from this study is that excessive lateralization may introduce unintended adverse effects when taken to the extreme. Planning should ideally include an assessment of tuberosity-acromion impingement (and potentially minimizing lateralization if an issue presents) and avoiding over-lateralizing with large glenoid augments or lateralized sphere’s; particularly in female patients when using a lateral humerus onlay constuct. These individuals may be at risk of acromial strain or fracture, which is one hypothesis as to why this cohort had lower outcome scores in this study.
Future Role of AI in Optimizing Implant Position
Perhaps someday patient factors and the CT scan can be placed into an artificial intelligence algorithm and based on the prosthesis planned, recommendations can be made for precise implant position and size on the humerus and glenoid. Until then, surgeons should scrutinize their preoperative 3D CT plans, consider using imaging variables such as the DSA and LSA to optimize implant position, ensuring optimal impingement-free range of motion, while minimizing over lateralization that can lead to deleterious outcomes, like the ones observed in this study.